IPA Priorities
Independent Physician Associations (IPAs) are stepping in to provide support as physician-led entity groups enable providers to flex their muscle collectively
IPA Value-Based Care Opportunity
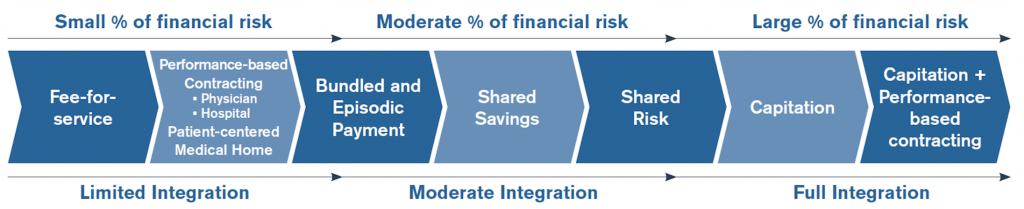
Accelerating moves toward increased risk responsibility compensation and Value-Based Healthcare is rapidly expanding the demand for Managed Care Service Providers with expertise in delegated care contracting and care delivery. MHM Health assists organizations evolve and transform into the type of network required to succeed in the opportunities and avoid the pitfalls that lie ahead.
Whether you are an existing IPA wanting to evolve and expand risk participation and or you want to build a new Managed and Value-Based Care network, MHM Health is uniquely able to design, build, and operate comprehensive network to enable growth and maximize patient outreach to support shared savings and risk-based contracts.
- We assess provider-network readiness to participate in the higher quality care, clinical performance, utilization, cost, and value demanded by payors
- We provide the experienced people, the programs, the processes, and the technologies which elevate provider-network capabilities and performance.
- We operate the foundation Quality, Medical Management, and Risk Revenue Management services required for accountable care
- Enable and position provider-network to successfully participate in new payer value-based care and payment models
Together we will: understand the capabilities required to exceed payer requirements.
- Analyze payor risk model and contract options
- Identify required care network capabilities and gaps
- Inventory current medical management and operational capabilities
- Formalize provider performance development, training, and support requirements